This week I was the one who broke one of the big nursing home "rules." I was the visitor who let a resident leave a locked unit.
I was covering for a colleague, visiting a dying patient in a nursing home that I don't normally cover. Although I used to be a chaplain in the building, I'm not the chaplain now so I'm not familiar with the residents; I only know the staff. As I was leaving the floor, I caught up to a gentleman who had just reached the elevator. I looked at him as I fumbled around trying to figure out how the elevator worked. (It used to have a nice covering over the "down" button so you had to use your keys or a pen through the grill to press the button. Now there is a full covering and a small metal piece on a chain that "locks" it in place. You have to pull out the metal piece, lift the cover and press the button, then close the cover and replace the metal piece. I got the metal piece out, but didn't know to lift the cover, so I was jabbing the metal piece every which way until I figured it out.)
While wondering if I was going to have to go to the nurse's station and get help with elevator instructions, I assessed the gentleman. He wore nice trousers and a long-sleeved white button-down shirt. He was shaved and his hair was combed. There was no noticeable wristband or ankle bracelet. There was minimal conversation, but we didn't know each other. Resident or family member? There was no way to tell. I've met a lot of men his age who come daily or twice a day to visit their wives on the dementia unit and he looked more put together than many of them.
So when he got into the elevator with me, I didn't ask if he was supposed to be there. (There's really no polite way - "Excuse me. Do you have dementia?" "Are you allowed off the floor?") But there must have been something, because when I got off the elevator I thought, "I should check with a staff member."
There was no need. Almost immediately a staff member assisting another resident looked at him and asked, "'Bob.' What are you doing here?" Another came and gently took his arm, "Here, let's go this way." And another, "What's 'Bob' doing off the floor?"
Today, when I again visited that nursing home, I was greeted (among other things) with, "I hear you let 'Bob' off the floor yesterday." I apologized. They laughed. I have the feeling that this happens often with 'Bob.'
In many of the nursing homes I visit there's a resident who doesn't quite seem to belong on the floor. Someone who is still walking around; someone who remembers the social graces and can provide polite chit-chat. Perhaps it's someone who is no longer safe living alone. Or a person whose family can no longer provide the amount of care they need. I've met many family members, especially spouses, who have run their own health into the ground while caring for a loved one with dementia, until the needs become too great and a nursing home or assisted living is the best option.
And I've met residents who ask me to "get me out of here." One wants me to gather up her medical records "RIGHT NOW" because she has "a medical appointment and needs the doctor to see" that she doesn't "belong on an Alzheimer's floor." Another wants me to call her lawyer. "You can see that I should be living on my own. My daughter put me here. She sold my car. She lives in the South. I have a cousin who will help me. I just need you to call." I always talk to the staff. Again and again I speak with residents (not my patients) who present well and just want my help to "go home." I know that they are no longer capable of caring for themselves (and I've asked.) I know some of the stories. And it breaks my heart that I can't help them (and that they can't remember that I can't help them, so they repeat the request the next time they see me and the next.) Some days the hardest part of my job isn't the hospice patients.
But the next time I'm waiting for the elevator (or struggling to circumvent the lock that keeps the residents in,) I'm going to take a second and a third look at those people who are waiting with me!
Tuesday, September 28, 2010
Friday, September 17, 2010
Again with the shofar
I had the shofar with me today. A Jewish patient who was not inclined to hear it a few weeks ago - he had other things on his mind that day, and didn't recognize the shofar - said "yes," he'd enjoy hearing it. So I let everyone around know what I would be doing and then blew a mighty "tekiya."
"You shouldn't do that when you're crossing the street," he told me. "Too many people might get hurt."
"You shouldn't do that when you're crossing the street," he told me. "Too many people might get hurt."
Thursday, September 16, 2010
Driving down the highway . . .
It's been one of those weeks.
I've driven between 70 and 90 miles each day this week Normally I try to schedule my day so that the facilities I visit are near each other. But with Holy Days, new admissions, visits that had to be made this week, and patients who were not doing well, I was going from one end of my territory to the other - every day.
This time of the year, however, I like long car rides. I use the time for Yom Kippur preparation. Not for work - but for me. I listen to podcasts - programs like "Speaking of Faith" that either have specific High Holy Day programs or programs that are thematically linked to the Holy Days. I listen to music. The sounds of "Avinu Malchenu" and "U'nitanah Tokef" fill my car (and I turn the sound up, and sometimes hit the "repeat" button.)
As I drive I reflect on the ways I can be better and do better in the New Year. I think about my family and friends. I remember people who we lost in the old year. Often when I reach the nursing home I'm visiting, I spend a few extra minutes in the car listening to the end of a song or a section of a podcast.
Sometimes a word or phrase or musical piece reminds me of a book I recently read, or a sermon I heard, or some aspect of the holidays I've been ruminating over. I become lost in thought and the words or music become a muted background to my own thoughts. So far, and somewhat surprisingly, I've managed all this without missing my exit or getting lost.
It's been one of those weeks. But this week I've been happy to have the extra time on the road, as all the roads I've traveled have led me back to myself and forward to atonement.
I've driven between 70 and 90 miles each day this week Normally I try to schedule my day so that the facilities I visit are near each other. But with Holy Days, new admissions, visits that had to be made this week, and patients who were not doing well, I was going from one end of my territory to the other - every day.
This time of the year, however, I like long car rides. I use the time for Yom Kippur preparation. Not for work - but for me. I listen to podcasts - programs like "Speaking of Faith" that either have specific High Holy Day programs or programs that are thematically linked to the Holy Days. I listen to music. The sounds of "Avinu Malchenu" and "U'nitanah Tokef" fill my car (and I turn the sound up, and sometimes hit the "repeat" button.)
As I drive I reflect on the ways I can be better and do better in the New Year. I think about my family and friends. I remember people who we lost in the old year. Often when I reach the nursing home I'm visiting, I spend a few extra minutes in the car listening to the end of a song or a section of a podcast.
Sometimes a word or phrase or musical piece reminds me of a book I recently read, or a sermon I heard, or some aspect of the holidays I've been ruminating over. I become lost in thought and the words or music become a muted background to my own thoughts. So far, and somewhat surprisingly, I've managed all this without missing my exit or getting lost.
It's been one of those weeks. But this week I've been happy to have the extra time on the road, as all the roads I've traveled have led me back to myself and forward to atonement.
Tuesday, September 14, 2010
Happy . . . Hanukah ? ?
One of the residents at a facility I visit is always happy to see me. "I love you, I love you," she has told me. She met me when I was her brother's hospice chaplain in the the same facility. I am grateful that she doesn't connect me with her loss or see me as a reminder of her sorrow.
Initially she recognized me by my kipah, now she recognizes me as me. Whenever she sees me, she gives me the appropriate Jewish greeting (or at least the Jewish greeting she knows.) "Happy Hanukah," she says. "Happy Hanukah." I thank her.
I saw her last week, just before Rosh HaShanah. She wished me a "Happy Hanukah."
I couldn't help noticing that the local Chabad has their hanukiya fully lit for their New Year observances. Perhaps she's right: it's always hanukah somewhere.
Initially she recognized me by my kipah, now she recognizes me as me. Whenever she sees me, she gives me the appropriate Jewish greeting (or at least the Jewish greeting she knows.) "Happy Hanukah," she says. "Happy Hanukah." I thank her.
I saw her last week, just before Rosh HaShanah. She wished me a "Happy Hanukah."
I couldn't help noticing that the local Chabad has their hanukiya fully lit for their New Year observances. Perhaps she's right: it's always hanukah somewhere.
Wednesday, September 8, 2010
Tales of the shofar
The shofar's out of the cupboard and into my workplaces. So far:
My patient's eyes are open when a greet her - a rarity - perhaps due to the lunch-time visit. I greet her and mention the New Year. Her eyes close. I sound the shofar - the whole series - loudly. No reaction from her; her eyes remain closed. But the gentleman next to her turns to me and asks: "What the hell was that??!!"
I do a "service" for a nursing home with a younger population. Some sing along with "Avinu Malcheinu." Some "talk back" at me during the story (I love that!) We listen to Kol Nidre. And during the course of the service I sound the shofar. They are so appreciative. I get to go around the room afterward and everyone wants to shake my hand and wish me a "happy new year." And I shake all of their hands and wish them a "happy and blessed year" as well. It's a good thing that State isn't here to chastise me for not washing my hands in between every handshake. It may not meet universal precautions, but the moment and the touch far outweigh the benefit of trying to follow the letter of the law in this case.
I ask one of my facilities if they have any Jewish residents who would like to hear the shofar. "The only people we've ever seen in the building with a yarmulke are you and that examiner from the State. He hasn't been around lately." "Ok, thanks. I didn't think you had any Jewish residents, but I always like to ask." "What does it sound like? Will you blow it for us?" So I do.
I give the activity director of another facility a CD of High Holy Day music for her Jewish resident (not one of my patients.) "Thank you so much. I'll put it in her room. Her family will be so glad to hear you came by." So . . . out comes the shofar and with a few introductory remarks to the staff, family and patients present, I blow the shofar. The Jewish resident gives me a little smile. "Please let her family know that I also brought in the shofar so she could hear it."
My office thinks of it as good PR and outreach. I think of it as a mitzvah and my preparation for entering the Holy Days.
שנה טובה ומתוקה
May we all be blessed with a sweet and good New Year.
My patient's eyes are open when a greet her - a rarity - perhaps due to the lunch-time visit. I greet her and mention the New Year. Her eyes close. I sound the shofar - the whole series - loudly. No reaction from her; her eyes remain closed. But the gentleman next to her turns to me and asks: "What the hell was that??!!"
I do a "service" for a nursing home with a younger population. Some sing along with "Avinu Malcheinu." Some "talk back" at me during the story (I love that!) We listen to Kol Nidre. And during the course of the service I sound the shofar. They are so appreciative. I get to go around the room afterward and everyone wants to shake my hand and wish me a "happy new year." And I shake all of their hands and wish them a "happy and blessed year" as well. It's a good thing that State isn't here to chastise me for not washing my hands in between every handshake. It may not meet universal precautions, but the moment and the touch far outweigh the benefit of trying to follow the letter of the law in this case.
I ask one of my facilities if they have any Jewish residents who would like to hear the shofar. "The only people we've ever seen in the building with a yarmulke are you and that examiner from the State. He hasn't been around lately." "Ok, thanks. I didn't think you had any Jewish residents, but I always like to ask." "What does it sound like? Will you blow it for us?" So I do.
I give the activity director of another facility a CD of High Holy Day music for her Jewish resident (not one of my patients.) "Thank you so much. I'll put it in her room. Her family will be so glad to hear you came by." So . . . out comes the shofar and with a few introductory remarks to the staff, family and patients present, I blow the shofar. The Jewish resident gives me a little smile. "Please let her family know that I also brought in the shofar so she could hear it."
My office thinks of it as good PR and outreach. I think of it as a mitzvah and my preparation for entering the Holy Days.
שנה טובה ומתוקה
May we all be blessed with a sweet and good New Year.
Tuesday, September 7, 2010
The unexpected . . . or what teenagers taught me about conversation
Some days hospice work bears a certain resemblance to working with teenagers. Anyone who has worked with (or had) teenagers knows that some of the best conversations you have are the ones that take place in the car. Whether it's the forced intimacy or the lack of eye contact, or just serendipity, a car ride can turn into an unexpected opportunity for sharing. Something special can take place in that moment. You can't plan for it or expect it or extend it. You can only experience it and give thanks for it.
Some days you have moments like that in hospice. Again, you can't plan it and you can't force it. And just because you had that special moment once with a patient or family, you can't expect it to happen again.
Much like moments in the car, some of these moments happen when I am not looking at my patient. This week I was sitting with a patient who does not talk a lot. He does like it, however, when the social worker or I sit quietly next to him and do our paperwork. He likes the company and the companionship.
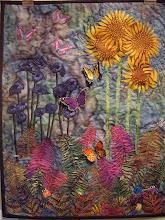
The other day I sat next to him with a big afghan on my lap. The afghan belonged to another patient. It had been lost and then found in the laundry by a facility CNA. The yarn had broken in some places, been pulled out in others, and had open stitches that were unraveling. I had told the CNA that I would try to fix it. (Fortunately I usually carry knitting and had both a crochet hook and a yarn needle in my car.)
So I sat next to my patient and focused my attention on the yarn and the open stitches. I don't know whether it was my attention to the task, my awareness of some of his issues and concerns, or my thoughts focusing on Elul, but as I talked with him about what I was doing it turned into one of those unplanned, special moments.
I commented that it could be a challenging task to try to fix something that had been torn or broken. "Yes," he said. I sewed some more and said, "I know I can't make this perfect, but at least I can mend some of the holes and keep it from getting worse." He agreed. Although he's not much of a talker, I realized he was very focused on my words and actions. So I continued to mend the afghan and talk about repairing the things we could, letting go of the things we couldn't, and forgiving ourselves for not being perfect. He would listen, make a tiny comment or a sound of acknowledgment. This continued until there was no more yarn to reattach.
I know that I got a great deal out of this unexpected moment and conversation. I think that he did as well, for I have an invitation to visit again . . . and to bring my knitting.
Some days you have moments like that in hospice. Again, you can't plan it and you can't force it. And just because you had that special moment once with a patient or family, you can't expect it to happen again.
Much like moments in the car, some of these moments happen when I am not looking at my patient. This week I was sitting with a patient who does not talk a lot. He does like it, however, when the social worker or I sit quietly next to him and do our paperwork. He likes the company and the companionship.
The other day I sat next to him with a big afghan on my lap. The afghan belonged to another patient. It had been lost and then found in the laundry by a facility CNA. The yarn had broken in some places, been pulled out in others, and had open stitches that were unraveling. I had told the CNA that I would try to fix it. (Fortunately I usually carry knitting and had both a crochet hook and a yarn needle in my car.)
So I sat next to my patient and focused my attention on the yarn and the open stitches. I don't know whether it was my attention to the task, my awareness of some of his issues and concerns, or my thoughts focusing on Elul, but as I talked with him about what I was doing it turned into one of those unplanned, special moments.
I commented that it could be a challenging task to try to fix something that had been torn or broken. "Yes," he said. I sewed some more and said, "I know I can't make this perfect, but at least I can mend some of the holes and keep it from getting worse." He agreed. Although he's not much of a talker, I realized he was very focused on my words and actions. So I continued to mend the afghan and talk about repairing the things we could, letting go of the things we couldn't, and forgiving ourselves for not being perfect. He would listen, make a tiny comment or a sound of acknowledgment. This continued until there was no more yarn to reattach.
I know that I got a great deal out of this unexpected moment and conversation. I think that he did as well, for I have an invitation to visit again . . . and to bring my knitting.
Sunday, September 5, 2010
Sitting & knitting
We have a new patient. She's in her 90's. The family says she's "given up," she's "ready to go." The family is clearly not ready to let her go. They're willing to talk hospice, but they are hoping that the extra attention and services will tip her back on the side of living. I ask about volunteers. "She knits," they say. "Do you have someone who could come knit with her and maybe also pick up the stitches she drops?" "I knit," I say. "I'll see what I can do."
At my initial, and as it turns out, only, visit with the patient, she's curled up in the middle of her bed with the covers pulled up to the top of her head. She doesn't respond to my greeting or presence. So I sit down next to the bed, pull out my knitting, and knit. Eventually she says a word or two. As I sit there, a younger woman comes in. She's the daughter of another resident, a friend of my patient, a knitting companion. The younger woman and I talk about knitting. And then a voice comes from under the covers: "I think I'm dying."
Before I can even open my mouth to respond, possibly faster than the speed of light, the other woman says, "Oh no. You're not dying. You just need to eat more." My thoughts are unprintable. Eventually the other woman leaves. I continue to knit. And knit.
Finally I say, "So you think you're dying. What makes you think that?" She says, "I just don't feel well." She's silent and I knit some more.
Finally she says, "Am I dying?" I take a deep breath. "Everyone dies sooner or later . . . I think for you it will be sooner. You're not eating and you tell me that you just don't feel well." More silence. I've answered her question. I've told her what she needs to hear. She doesn't say anything else.
And a few days later she dies.
At my initial, and as it turns out, only, visit with the patient, she's curled up in the middle of her bed with the covers pulled up to the top of her head. She doesn't respond to my greeting or presence. So I sit down next to the bed, pull out my knitting, and knit. Eventually she says a word or two. As I sit there, a younger woman comes in. She's the daughter of another resident, a friend of my patient, a knitting companion. The younger woman and I talk about knitting. And then a voice comes from under the covers: "I think I'm dying."
Before I can even open my mouth to respond, possibly faster than the speed of light, the other woman says, "Oh no. You're not dying. You just need to eat more." My thoughts are unprintable. Eventually the other woman leaves. I continue to knit. And knit.
Finally I say, "So you think you're dying. What makes you think that?" She says, "I just don't feel well." She's silent and I knit some more.
Finally she says, "Am I dying?" I take a deep breath. "Everyone dies sooner or later . . . I think for you it will be sooner. You're not eating and you tell me that you just don't feel well." More silence. I've answered her question. I've told her what she needs to hear. She doesn't say anything else.
And a few days later she dies.
Subscribe to:
Posts (Atom)